With CY 2021 Medicare Advantage deadlines rapidly approaching, state Medicaid agencies and Medicare Advantage plans offering Dual Eligible Special Needs Plans must quickly determine how to fulfill new integration requirements mandated by the Bipartisan Budget Act of 2018.
This white paper summarizes the new requirements and discusses stakeholder considerations.
Background
Dual eligible special needs plans (D-SNPs) are Medicare Advantage (MA) plans that only enroll beneficiaries who are dually eligible for Medicare and Medicaid. D-SNPs have become increasingly popular among both MA organizations (MAOs) and dual eligible beneficiaries because of their ability to tailor benefit designs to the needs of this population. Approximately one-quarter of the nation’s 11 million dual eligible beneficiaries are enrolled in one of the 550+ D-SNPs offered throughout the country as of January 2020. 1,2 Figure 1 shows the proportion of dual eligible beneficiaries, by state, enrolled in D-SNPs as of January 2020.
In addition to limiting enrollment to dual eligible beneficiaries, D-SNPs are required to have a model of care approved by the National Committee for Quality Assurance (NCQA) and a state Medicaid agency contract (SMAC) or a Medicare Improvements for Patients and Providers Act (MIPPA) contract. The SMAC outlines various contractual and integration details such as dual eligible categories eligible for enrollment (e.g., full duals, partial duals, Qualified Medicare Beneficiaries) and Medicaid benefits to be covered by the D-SNP, if any. 3 Each state Medicaid agency has the authority to define the terms in the SMAC and decide which MAOs it permits to offer D-SNPs within the state.
Figure 1: D-SNP penetration by state (January 2020)
New requirements from CMS
Beginning in calendar year (CY) 2021, D-SNPs will be required to meet new minimum integration standards through at least one of the following avenues, as seen in Figure 2.4,5
-
OBTAIN FULLY INTEGRATED DUAL ELIGIBLE (FIDE) SNP STATUS
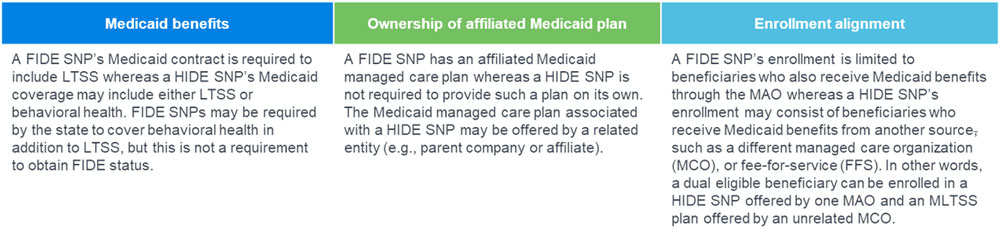
FIDE SNPs are integrated plans that provide both Medicare and Medicaid benefits, including long-term services and supports (LTSS), to enrolled beneficiaries. FIDE SNPs have an MA contract with the Centers for Medicare and Medicaid Services (CMS) and a Medicaid managed care contract with the state Medicaid agency. FIDE SNPs were enacted by the Patient Protection and Affordable Care Act (ACA) and currently comprise about 11% of current D-SNP enrollment - OBTAIN HIGHLY INTEGRATED DUAL ELIGIBLE (HIDE) SNP STATUS
HIDE SNPs are MA plans that are offered by an MAO that itself offers a separate Medicaid managed LTSS (MLTSS) plan or a Medicaid managed behavioral health plan within the D-SNP service area, or that has a related entity offering such a managed care plan. HIDE SNP is a new designation defined by the Bipartisan Budget Act of 2018, and no such plans currently exist. - ESTABLISH A PROCESS TO NOTIFY THE STATE OR A STATE DESIGNEE OF HOSPITAL OR SKILLED NURSING FACILITY ADMISSIONS FOR AT LEAST ONE GROUP OF HIGH-RISK ENROLLEES
D-SNPs that do not obtain FIDE SNP or HIDE SNP status must, in conjunction with the state, establish a process to notify the state when certain high-risk enrollees are admitted to a hospital or skilled nursing facility. The establishment and specifics of such a process are at the state’s discretion. Thus, some states could forgo this third option and only allow D-SNPs that obtain FIDE SNP or HIDE SNP status.
As the CY 2021 MA bid submission deadline approaches, state Medicaid agencies and MA plans offering D-SNPs must quickly determine how to fulfill the new D-SNP integration requirements.
Figure 2: CY 2021 D-SNP integration options
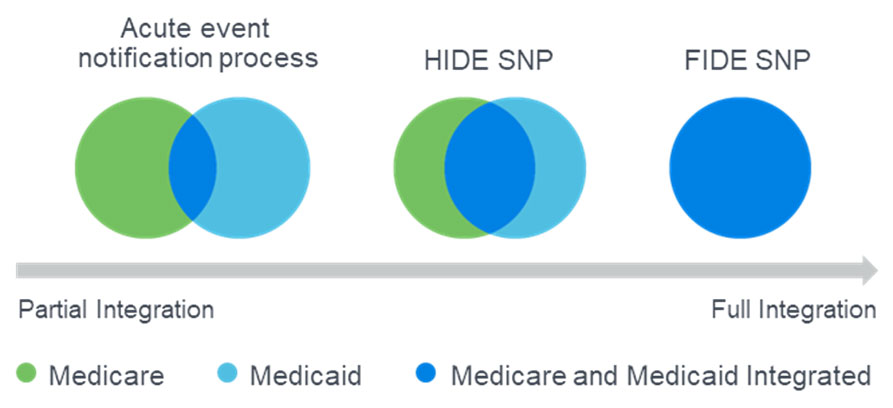
Figure 3: FIDE VS. HIDE distinction
Considerations for state Medicaid agencies
- STATES CONTROL INTEGRATION OPTIONS AVAILABLE TO MA ORGANIZATIONS
State Medicaid agencies have the authority to decide which organizations can offer D-SNPs and what types of D-SNPs are permitted in the state. Thus, states should be proactive and purposeful about how they intend D-SNPs to meet the new integration requirements. States should consider which of the new integration requirements best support current state objectives and they may want to consider different requirements in the short- and long-term. - ESTABLISHING AN INFORMATION-SHARING PROCESS COULD PRESENT OPERATIONAL HURDLES
Establishing a process for notification of hospital or skilled nursing facility admissions could require significant time and resource investment by both states and MAOs offering D-SNPs. Such a process would require coordination between states and MAOs, some of which may have no existing relationship with the state Medicaid agency. Establishing an information-sharing process may require cross-departmental collaboration including information technology (IT), claims processing, legal, clinical, and others. - REQUIRING FIDE SNP OR HIDE SNP STATUS COULD CAUSE MA MARKET DISRUPTION
Some states may consider only allowing FIDE or HIDE SNPs either to achieve integration goals or to avoid the administrative burden of establishing an information-sharing process with MAOs. This approach could result in MA market disruption if existing D-SNPs are unable to obtain FIDE or HIDE status by 2021 due to the lack of a Medicaid MLTSS or managed behavioral health plan. It could even result in an elimination of D-SNPs in states without existing Medicaid MLTSS or managed behavioral health programs. Even in states that require Medicaid MLTSS plans to offer companion D-SNPs, some existing D-SNPs may not have a companion MLTSS plan. MAOs that are unable to satisfy integration requirements may attempt to offer D-SNP look-alike plans. D-SNP look-alike plans are general enrollment MA plans that have similar plan designs as D-SNPs, but do not satisfy D-SNP model of care, SMAC, or integration requirements. CMS has expressed concern about D-SNP look-alikes and has proposed banning them beginning in CY 2022. 7 - D-SNP BID SUBMISSION DEADLINE IS JUNE 1, 2020
MAOs must file CY 2021 MA bids with CMS by June 1, 2020, and many have already begun the MA bid development process. States should engage with MAOs soon to communicate their approaches to meeting the integration requirements, to understand MAOs’ abilities to meet the new requirements, and to update SMACs. MAOs will need sufficient time to implement necessary changes and reflect the impact of changes in filed bids. - REASSESS DUAL INTEGRATION VISION
State Medicaid agencies may use the new integration requirements as an opportunity to gather input on broader dual integration vision and goals. Such discussions could guide near-term decisions regarding CY 2021 D-SNP integration requirements as well as longer-term programmatic considerations. Considerations may include the following: - Should the state’s D-SNP integration requirements evolve over time to achieve different goals or handle different timing constraints?
- Which dual eligibility classes are most effectively managed in D-SNPs?
- Are there enrollment mechanisms such as default enrollment that would enhance integration efforts?
- What is the state’s long-term strategy for managing LTSS costs?
- Should the state consider new fully integrated programs or revisions to existing programs such as FIDE SNPs, dual demonstrations, or the Program of All-Inclusive Care for the Elderly (PACE)?
- Should the state consider its own tailored approach to dual integration such as those outlined in the letter of April 24, 2019, to state Medicaid directors from CMS Administrator Seema Verma (SMDL #19-002)?8
Considerations for MAOs offering D-SNPs
- FIDE SNP OR HIDE SNP STATUS MAY NOT BE ATTAINABLE BY 2021
D-SNPs offered by MAOs without a Medicaid MLTSS or managed behavioral health plan (and whose parent organizations and related entities also lack such a plan) do not satisfy FIDE SNP or HIDE SNP requirements. MAOs in this situation may need to advocate for states to implement an information-sharing process, as it would be the only short-term way to satisfy the new integration standards. - STATES’ APPROACHES TO INTEGRATION MAY PROVIDE ENROLLMENT OPPORTUNITIES
If a state requires all D-SNPs to obtain FIDE SNP or HIDE SNP status, then any existing D-SNP offered by an MAO without a Medicaid MLTSS or managed behavioral health plan will be unable to meet the new integration standards. This could result in a reduction in the number of D-SNPs within a state, which would provide an opportunity for increased enrollment for existing FIDE and HIDE SNPs. It may also be an opportunity for D-SNP market entry for Medicaid MLTSS or behavioral health MCOs that do not currently offer a D-SNP. - ENGAGE WITH STATES AS SOON AS POSSIBLE
It is imperative that MAOs engage with their respective state Medicaid agencies as soon as possible to understand how each state intends D-SNPs to fulfill the new integration requirements. MAOs should determine whether significant plan changes (e.g., eligible dual classifications, service area) or administrative changes (e.g., hospital admission notification) will be required and reflect those changes in MA bids filed by June 1, 2020. All states and MAOs offering D-SNPs will need to update SMACs prior to the July 6 deadline. - ESTABLISHING AN INFORMATION-SHARING PROCESS COULD PRESENT OPERATIONAL CHALLENGES Establishing a process for notification of hospital or skilled nursing facility admissions could require significant time and resource investment across multiple internal departments (e.g., IT, actuarial, claims processing, legal, and clinical). MAOs will also need to collaborate with external parties (e.g., state Medicaid agencies, providers, other MAOs).
- REASSESS MEDICAID MANAGED CARE MARKET
Depending on a state’s approach to the new D-SNP integration requirements, operating a Medicaid MLTSS or managed behavioral health plan may be a barrier to entry into the D-SNP market. MAOs that are not currently in the Medicaid managed care market may want to consider a longer-term strategy of entering the Medicaid market in order to have access to dual eligible beneficiaries in the MA market.
Conclusion
As the CY 2021 MA bid submission and D-SNP SMAC deadlines approach, state Medicaid agencies and MAOs offering D-SNPs must quickly determine how to fulfill the new D-SNP integration requirements. This is an ideal time for states and MAOs to reconsider longer-term strategies around dual integration.
Limitations
The opinions stated in this article are those of the authors and do not represent the viewpoint of Milliman.
Guidelines issued by the American Academy of Actuaries require actuaries to include their professional qualifications in all actuarial communications. Nick Johnson, Chris Kunkel, and Annie Hallum are members of the American Academy of Actuaries and meet the qualification standards for sharing the information in this article. To the best of their knowledge and belief, this information is complete and accurate.
This information is intended to provide an overview of the new D-SNP integration requirements for state Medicaid agencies and Medicare Advantage plans. The list of considerations outlined in this article and the discussion of each consideration are not exhaustive. State Medicaid agencies and MAOs should give careful consideration to their own situations and determine how the new D-SNP integration requirements impact them. This information may not be appropriate, and should not be used, for other purposes.
Milliman does not intend to benefit and assumes no duty of liability to parties who receive this information. Any recipient of this information should engage qualified professionals for advice appropriate to its own specific needs.
1CMS. SNP Comprehensive Report – January 2020. Retrieved February 18, 2020, from https://www.cms.gov/research-statistics-data-and-systemsstatistics-trends-and-reportsmcradvpartdenroldataspecial-needs/snp-comprehensive-report-2020-01.
2CMS. MMCO Statistical and Analytic Reports. Retrieved February 18, 2020, from https://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/Analytics.
3Office of Assistant Secretary for Planning and Evaluation (April 8, 2019). Integrating Care Through Dual Eligible Special Needs Plans (D-SNPs): Opportunities and Challenges. Retrieved February 18, 2020, from https://aspe.hhs.gov/basic-report/integrating-care-through-dual-eligible-special-needs-plans-d-snps-opportunities-and-challenges.
4CMS (October 7, 2019). CY 2021 Medicare-Medicaid Integration and Unified Appeals and Grievance Requirements for Dual Eligible Special Needs Plans (D-SNPs). Medicare-Medicaid Coordination Office. Retrieved February 18, 2020, from https://www.arabhealthonline.com/content/dam/Informa/arabhealthonline/
en/downloads/AH19_INDUSTRY_OVERVIEW_v3.pdf.
5CMS (January 17, 2020). Additional Guidance on CY 2021 Medicare-Medicaid Integration Requirements for Dual Eligible Special Needs Plans (D-SNPs). Medicare-Medicaid Coordination Office. Retrieved February 18, 2020, from https://www.cms.gov/files/document/CY2021dsnpsmedicaremedicaidintegrationrequirements.pdf.
6SNP Comprehensive Report – January 2020, op cit.
7CMS (February 18, 2020). Contract Year 2021 and 2022 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicaid Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly. Retrieved February 21, 2020, from https://www.federalregister.gov/documents/2020/02/18/2020-02085/medicare-and-medicaid-programs-contract-year-2021-and-2022-policy-and-technical-changes-to-the.
8Verma, S. (April 24, 2019). Three New Opportunities to Test Innovative Models of Integrated Care for Individuals Dually Eligible for Medicaid and Medicare. CMS SMDL #19-002. Retrieved February 18, 2020, from https://www.medicaid.gov/sites/default/files/Federal-Policy-Guidance/Downloads/smd19002.pdf.
9CY 2021 Medicare-Medicaid Integration and Unified Appeals and Grievance Requirements for Dual Eligible Special Needs Plans (D-SNPs), op cit.