Introduction
Many state Medicaid agencies continue to express interest in value-based payment (VBP)1 for both fee-for-service (FFS) and managed care programs. However, what states refer to as value, where they want to ultimately end up with VBP, and how they want to get there vary widely. There is a dizzying array of VBP models, implementation approaches, and administrative structures to choose from. Before a state goes too far down the path of designing and implementing models, there are a few strategic decision points that require careful consideration to help set the state down the best path. This white paper is part of a Milliman series focused on considerations for state Medicaid agencies interested in increasing the adoption of VBP in their states. This first paper focuses on up-front strategic planning.
Start with the end in mind
VBP is a means to an end, so thinking up front about what the end should look like makes sense. The implications of neglecting to set objectives during strategic planning are multifaceted. An absence of clear priorities can lead to wasted resources while directionless efforts can lead to decreased motivation among stakeholders. Moreover, a lack of specific goal parameters can increase the difficulty in measuring success or progress. Contrariwise, having clear VBP goals from the beginning can guide design decisions and trade-offs when deciding which providers to hold accountable, identifying target population(s), selecting quality initiatives, and establishing risk-sharing parameters. Measurable VBP program objectives can help the monitoring of progress so the course can be corrected as needed. Although it is incredibly helpful to establish these goals, it can be daunting to get started. As such, it may be helpful to start with some high-level questions that can help define the scope and direction of the VBP strategy, including:
- What specific health outcomes are the stakeholders looking to drive? Some examples may include improving maternity outcomes, managing metabolic health, improving access and effectiveness of mental health, improving quality of care, reducing costs, or reducing hospital readmissions. Identify the populations in which there may be opportunities to close gaps in care or better allocate resources.
- Can the identified opportunities be quantified? Understanding whether opportunities can be quantified will be helpful to better understand and compare competing areas for focus.
- What are the priorities? While it may be tempting to go after all the opportunities identified, spreading resources too thin may undermine goals and efforts. Prioritization can consider the size of opportunities identified, anticipated room for improvement, likelihood of success, the available resources, and/or overall alignment with the Medicaid agency’s mission and vision.
- What metrics can be used to measure success? It is crucial to identify quantifiable and reliable indicators that can accurately reflect the progress toward the set goals. These metrics could include patient health outcomes, cost savings, or adherence to recommended care guidelines. The chosen metrics should be easily trackable over time and should align with the overall objectives of the VBP strategy.
- What funding is available? The amount of available funding may dictate the scope of VBP initiatives and program design. Some VBP programs can be designed to be revenue-neutral and therefore not require additional funding for provider reimbursement. However, the additional administrative costs of operating the VBP initiatives should always be considered.
- How will these goals evolve over time? VBP goals should be dynamic and adaptable. As the VBP initiatives progress and the healthcare landscape changes, it may be necessary to revise the goals to meet new challenges or opportunities. This could involve expanding the scope of the VBP program, incorporating new technologies or methodologies, or shifting focus to address emerging health issues within the target population. This evolution and pace of program changes should be guided by continuous monitoring and evaluation of the program's performance against its set objectives.
Thinking through these questions and answers can help with stakeholders’ alignment around program objectives, which maximizes the likelihood of program success.
Determine whether value-based payment will help achieve Medicaid program goals
VBP can be helpful for many program initiatives, but certainly not all initiatives. Most commonly, value-based payment is a useful solution when opportunities have been identified but current payment models are either a barrier or misalign incentives for stakeholders that can execute on that opportunity. In order to drive change in VBP there often needs to be a change in the way care is delivered. So when should states consider implementing a VBP model? One approach is to first identify opportunities for reducing spending or improving quality, and then identify care delivery changes needed to capture those opportunities. It is important to identify barriers to implementing care delivery changes throughout this process. The framework in Figure 1 may be helpful to assess population health or efficiency opportunities.
Figure 1: Assessing population health or efficiency opportunities

Some key elements in Figure 1 to be considered:
- Steps 2 and 3 are difficult to accomplish if the specific opportunity is not clearly identified. This illustrates the importance of goal-setting and identifying opportunities that support those goals.
- Step 2 is identifying the care delivery changes that need to take place to drive higher value.
- VBP is often a realignment of incentives, and sometimes a removal of barriers, to assist with driving changes in care delivery. Not all opportunities can be solved through payment changes. In practice it can often be a helpful component of a solution.
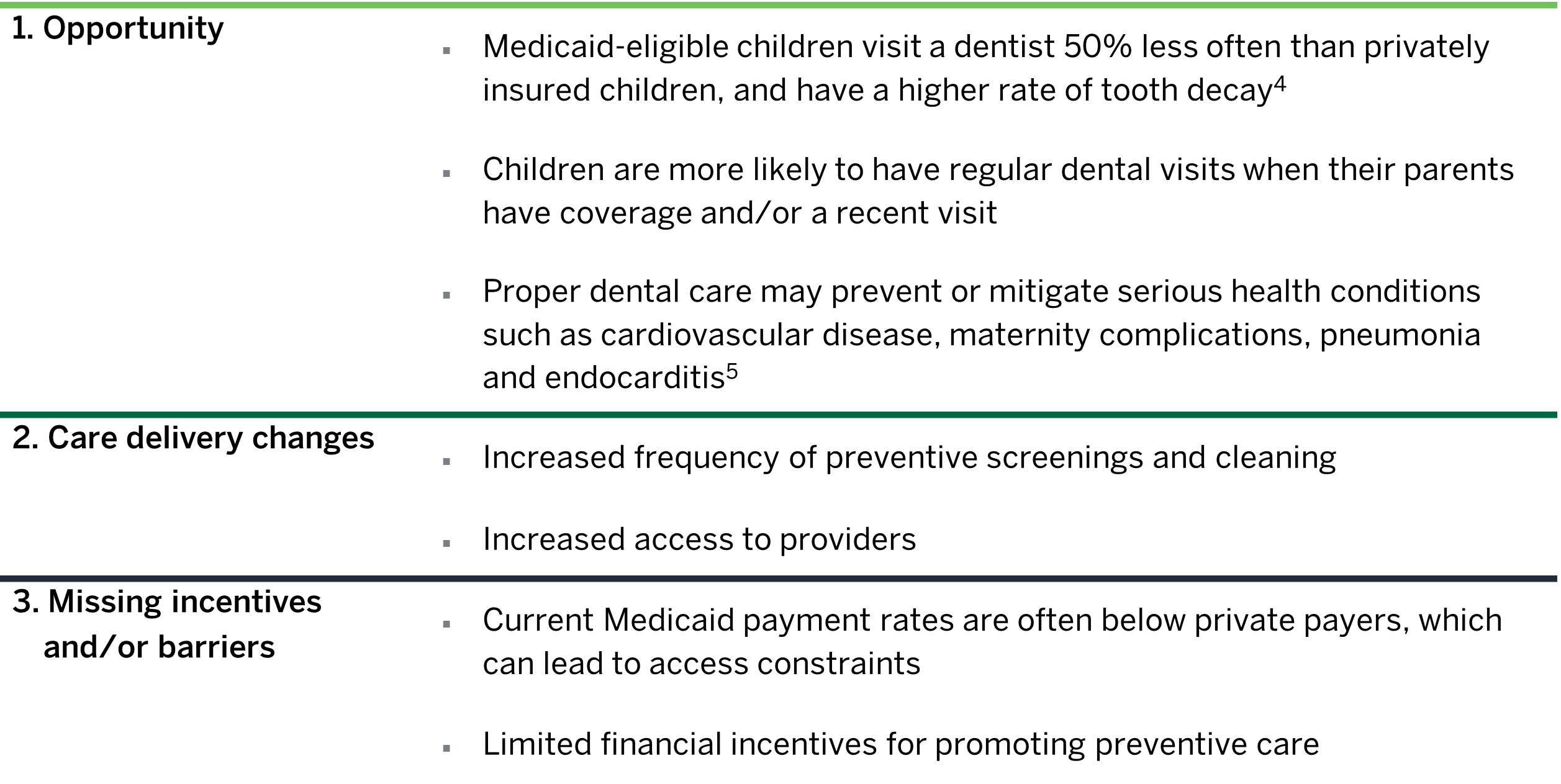
Figures 2 to 4 show three Medicaid-specific examples of how this framework can be applied to specific populations or services. These examples include maternity, health equity, and dental coverage. We specifically selected care delivery opportunities where traditional Medicaid fee-for-service payment models either present a barrier or do not provide incentives that facilitate the delivery of these high-value health services.
Figure 2: Maternity: Severe maternal mortality and morbidity (SMMM)2
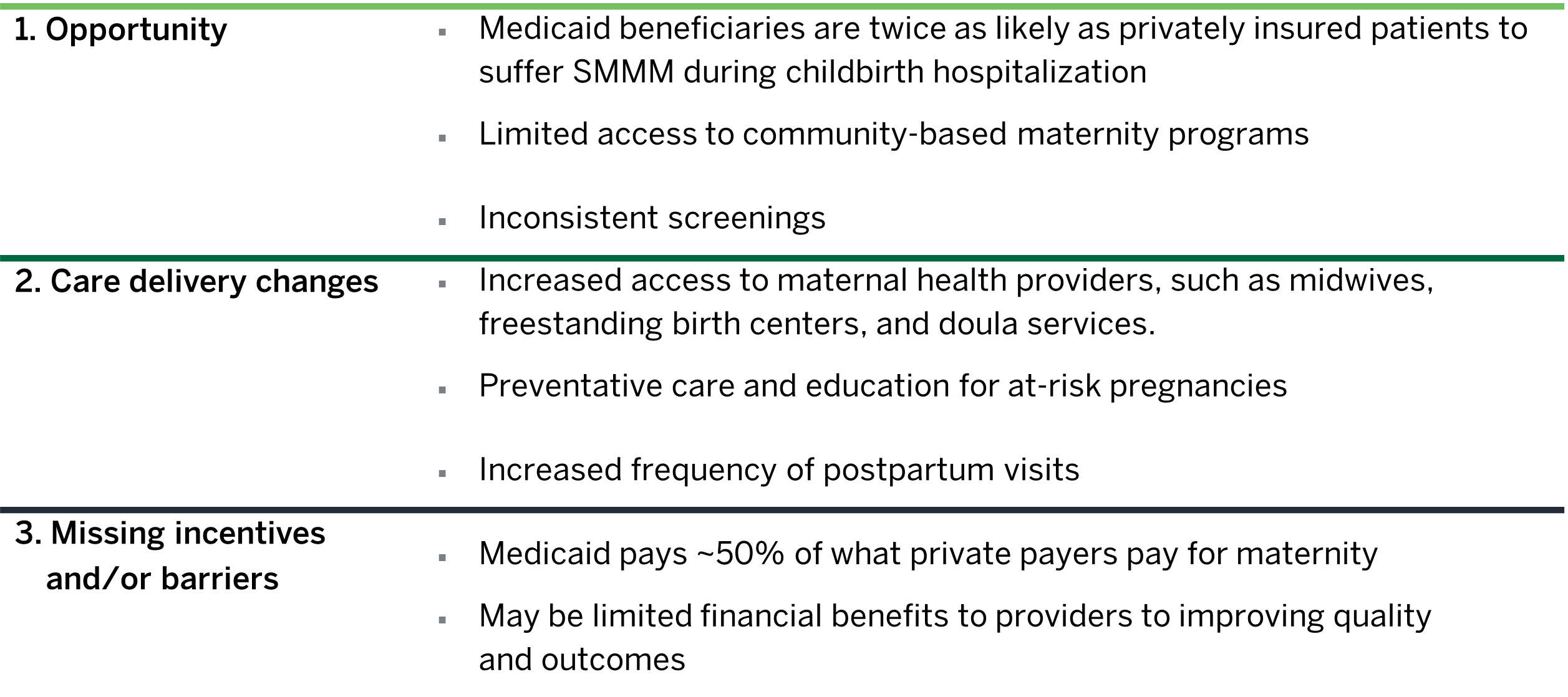
Figure 3: Health equity3
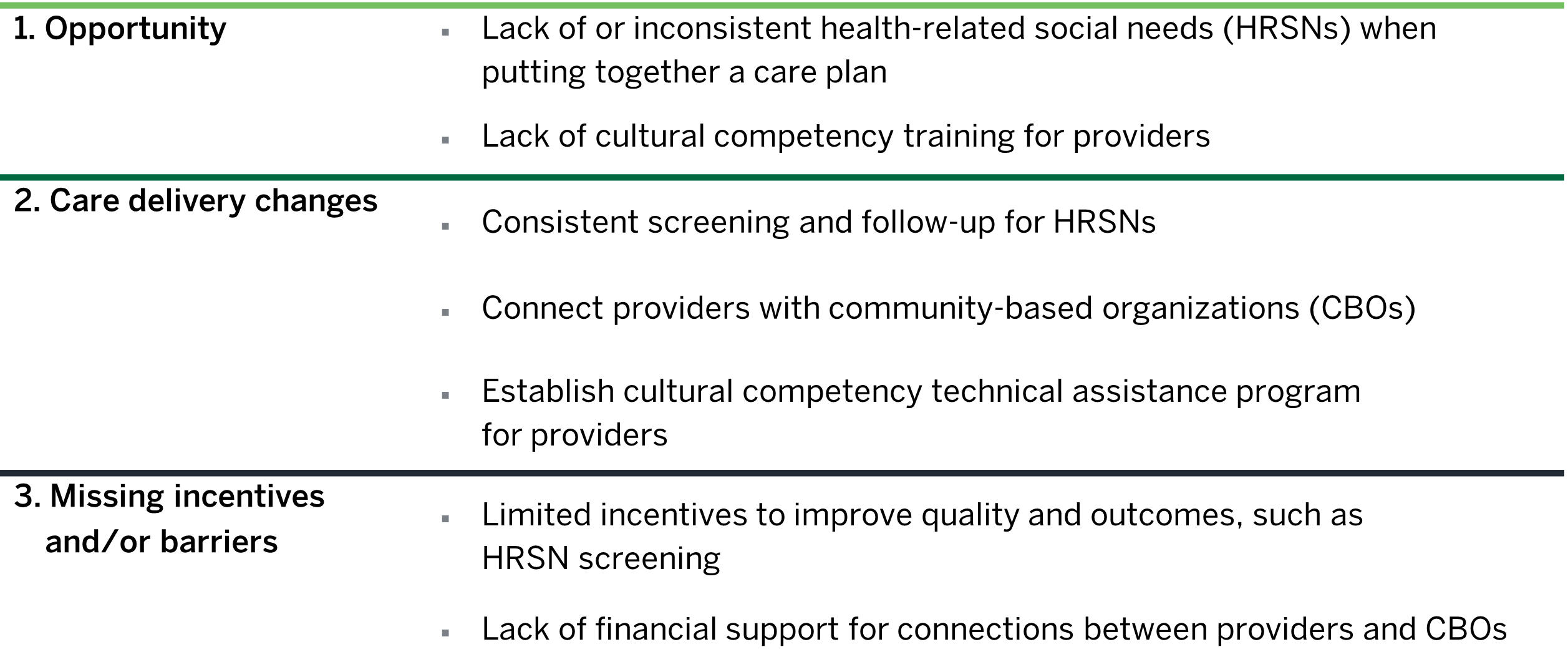
Figure 4: Dental care
The purpose of this phase in the strategic planning process is not to fully design a specific VBP model, which will require its own multi-phased process. Rather, the goal of this phase is simply to evaluate at a high level whether VBP is a relevant path to explore as a solution to some of the opportunities and goals identified up-front.
Consider the role the state Medicaid agency should play in rolling out value-based payment efforts
In managed Medicaid, driving value through payment design requires effort and participation from both the state and managed care organizations (MCOs). Often the description of a state's role in VBP efforts is simplified to either "state-directed or MCO-directed" or “directly or through guidance.” However, reality is more complex, with states' roles varying across and within different VBP initiatives. A simple framework that may be helpful for states to consider during the strategic planning process includes the following components: strategy, program design, implementation, and operations.
While some states may lean toward being prescriptive across all four areas and others lean toward being flexible across all areas, many states may prefer more control over certain aspects of the VBP program and allow flexibility for other aspects of the program. The role a state prefers could change over time, but it is important to be intentional up-front as this can have vast implications on the evolution, speed, and resource requirements for VBP adoption. Figure 5 provides examples showing how some states and MCOs have been leading these components. Because these steps are a continuum, there is some overlap from one component to the next.
Figure 5: Examples of state vs. MCO-directed processes
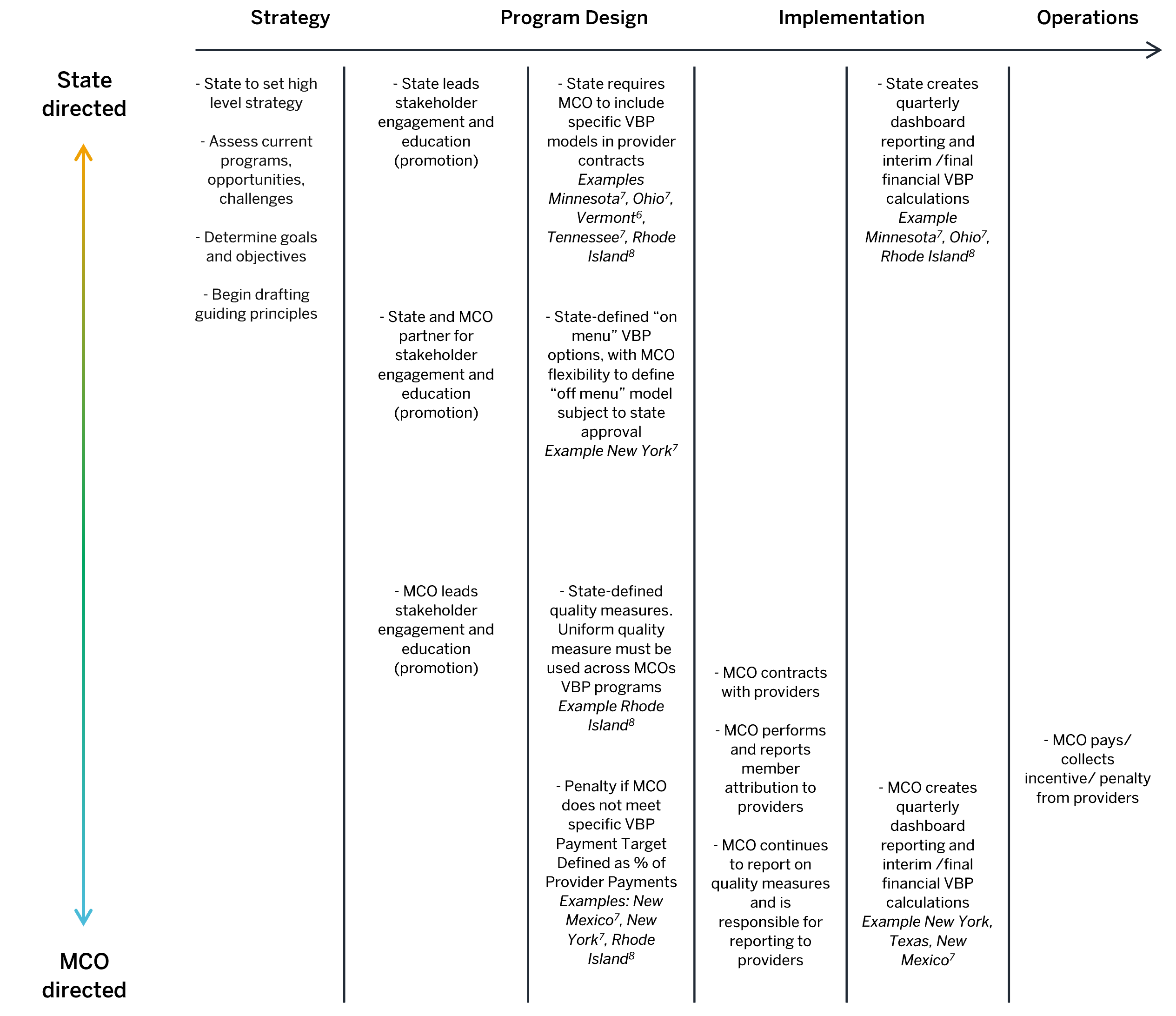
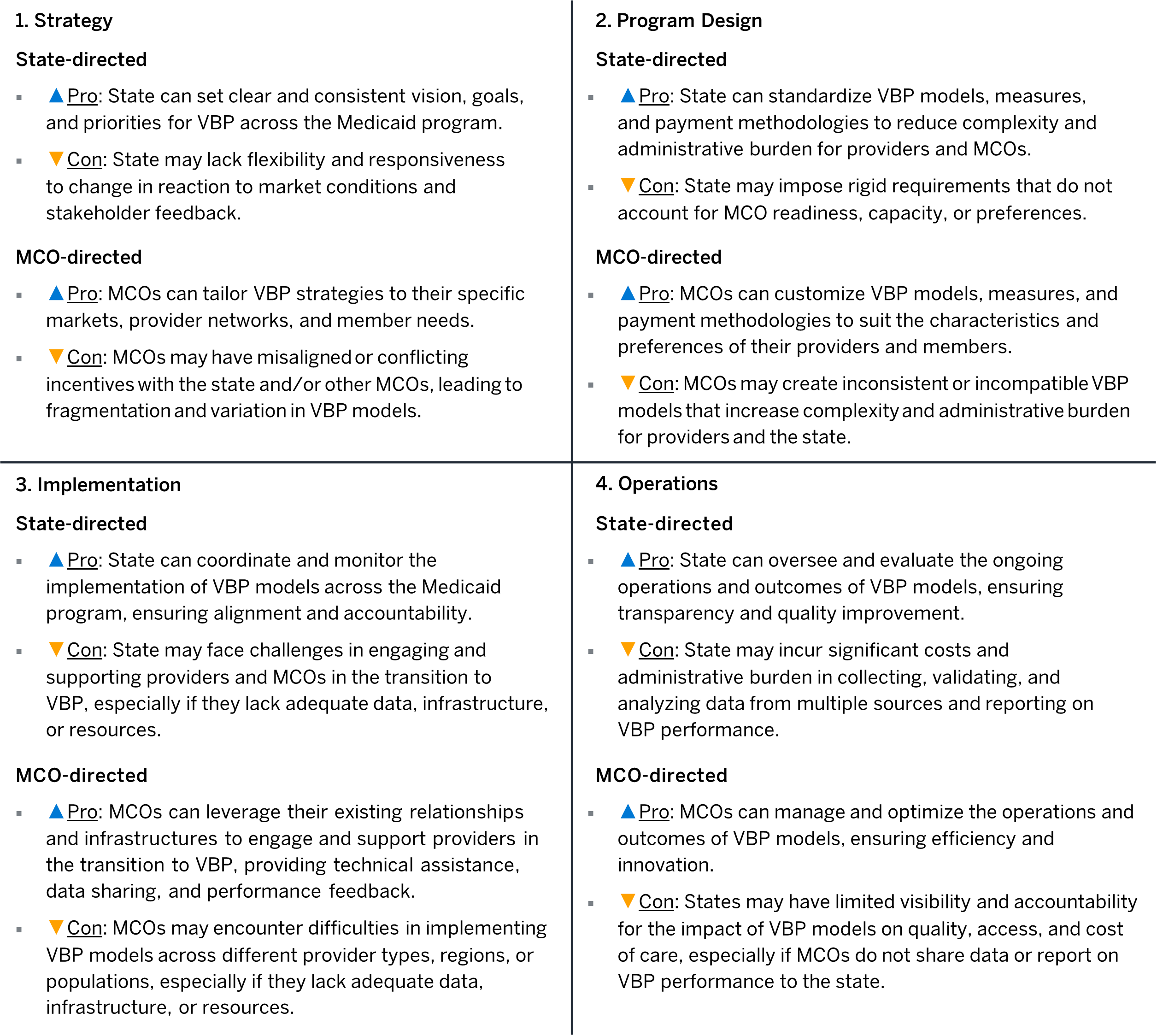
Figure 5 is neither comprehensive nor exhaustive but is intended to provide some examples. As states consider their role in a VBP program rollout, trade-offs arise with the various options. The ideal solution will vary depending on circumstances such as the state's goals, resources, and capabilities. The table in Figure 6 provides advantages and disadvantages of state-directed and MCO-directed approaches for each of the four VBP program components.
Figure 6: Advantages and disadvantages of VBP options
Conclusion
Although it is an up-front investment of time and energy, strategic planning on the part of the state is essential to ensuring success with VBP efforts. This includes careful consideration of the goals of the VBP program and the state’s role in the design, implementation, and ongoing operations of the programs. Each approach has its own advantages and challenges, and the best approach will depend on the specific circumstances of the state, MCOs, and providers involved. Many VBP programs aim to improve the quality of care for patients, ensure the financial viability of physician practices, and/or reduce spending for payers. By mapping out a deliberate plan and collaborating, all stakeholders can overcome the obstacles and achieve success in implementing VBP in the Medicaid environment.
1 Health Care Payment Learning and Action Network. Measurement Effort Results. Retrieved June 9, 2024, from https://hcp-lan.org/apm-measurement-effort/.
2 MACPAC (January 2000). Maternal Morbidity Among Women in Medicaid. Retrieved June 9, 2024, from https://www.macpac.gov/publication/maternal-morbidity-among-women-in-medicaid/.
3 Center for Health Care Strategies (May 2024). Building a Health Equity Focus Into Value-Based Payment Design: Approaches for Medicaid Payers. Retrieved June 9, 2024, from https://www.chcs.org/resource/building-a-health-equity-focus-into-value-based-payment-design-approaches-for-medicaid-payers/.
4 Finlayson T.L. et al. (2018).Child, caregiver, and family factors associated with child dental utilization among Mexican migrant families in California. Community Dent Health;35(2):89–94.
5 Mayo Clinic. Oral health: A window to your overall health. Retrieved June 9, 2024, from https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475.
6 Department of Vermont Health Access (2024). Vermont Medicaid Next Generation (VMNG) Accountable Care Organization (ACO) Program. Retrieved June 13, 2024, from https://dvha.vermont.gov/initiatives/payment-reform/vermont-medicaid-next-generation-aco-program.
7 Bailit Health (March 13, 2020). Final Report: State Strategies to Promote Value-Based Payment Through Medicaid Managed Care. Retrieved June 9, 2024, from https://www.macpac.gov/wp-content/uploads/2020/03/Final-Report-on-State-Strategies-to-Promote-Value-Based-Payment-through-Medicaid-Mananged-Care-Final-Report.pdf.
8 Rhode Island Executive Office of Health and Human Services (March 13, 2023). Accountable entities. Retrieved June 13, 2024, from https://eohhs.ri.gov/initiatives/accountable-entities.