Throughout the year, Milliman conducts regular Pulse Surveys focused on benefits topics that employers find meaningful and strategically informative. For this survey, we looked at a number of considerations that plan sponsors of health benefit plans are facing in light of the federal COVID-19 emergencies expiring on May 11, 2023.1 How are employers preparing for the end of these declared emergencies in regard to continuing certain coverages available during the pandemic, increased employee communications, or potential plan design decisions, including medical and behavioral health coverage such as employee assistance programs (EAPs)?
COVID-19 tests and testing-related services
Employers who sponsor health coverage will no longer be required to cover tests and testing-related services without cost sharing. Also, plans will no longer be required to cover over-the-counter (OTC) tests for plan participants.
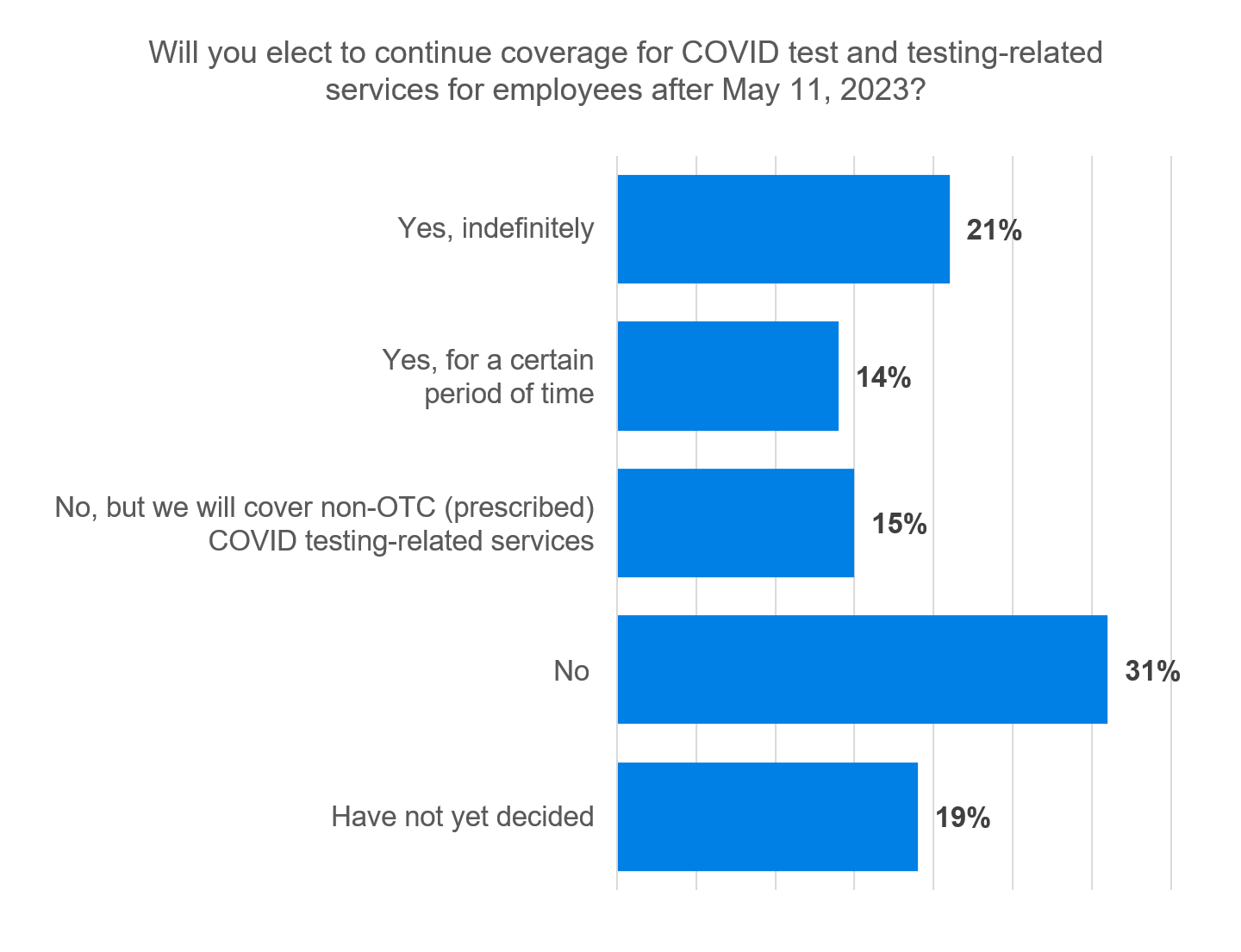
Most respondents (46%) indicated that they would not continue coverage for OTC COVID-19 tests and testing-related services.
Most of the respondents who said they are going to continue to cover testing haven’t considered a time limitation on that coverage. Twenty-one percent of respondents said they are going to cover testing and testing-related services indefinitely, whereas 14% indicated they would only continue coverage for a certain period of time.
Most surprising of all is that 19% of respondents stated they have yet to decide whether they are going to cover testing once the PHE is lifted. The significant amount of media and industry coverage about the lifting of the federal emergencies is what makes this result particularly interesting. There is a school of thought that the act of not making a decision is, in fact, making a decision.
There were several reasons why plan sponsors indicated they would elect to continue coverage. Thirty-two percent told us “it’s the right thing to do,” followed by 23% stating the cost of continuing coverage would be negligible. Another 14% cited the “high costs associated with those contracting COVID-19.”
Further, there was a clear correlation between the industry of the plan sponsor and choosing to extend coverage. For example, many plan sponsors in healthcare are choosing to extend coverage for the safety of patients and community residents. Plan sponsors in industries that were very much affected by closures as a result of pandemic measures, such as retail, hospitality, or arts and entertainment, were also choosing to extend testing coverage.
COVID-19 immunizations, including boosters
Under the Patient Protection and Affordable Care Act (ACA), employers that sponsor group health coverage will continue to be required to cover recommended preventive services2 (including immunizations) without cost sharing but can limit coverage to in-network providers. Interestingly, the survey results indicate that 39% of respondents are not choosing to limit covered vaccinations to just in-network providers.
Even though employers have had nearly five months to prepare for these expirations, a surprising number of respondents (41%) indicated they are taking a wait-and-see approach and haven’t made a decision on whether to limit vaccinations to in-network or not. This very well could be associated with the March 30, 2023, ruling of U.S. District Judge Reed O’Connor, which struck down the ACA mandate that insurers provide free preventive services, which took effect immediately. Carriers and plan sponsors alike are most likely awaiting guidance in light of the Biden administration’s appeal of this decision.
Telehealth benefits and remote care services
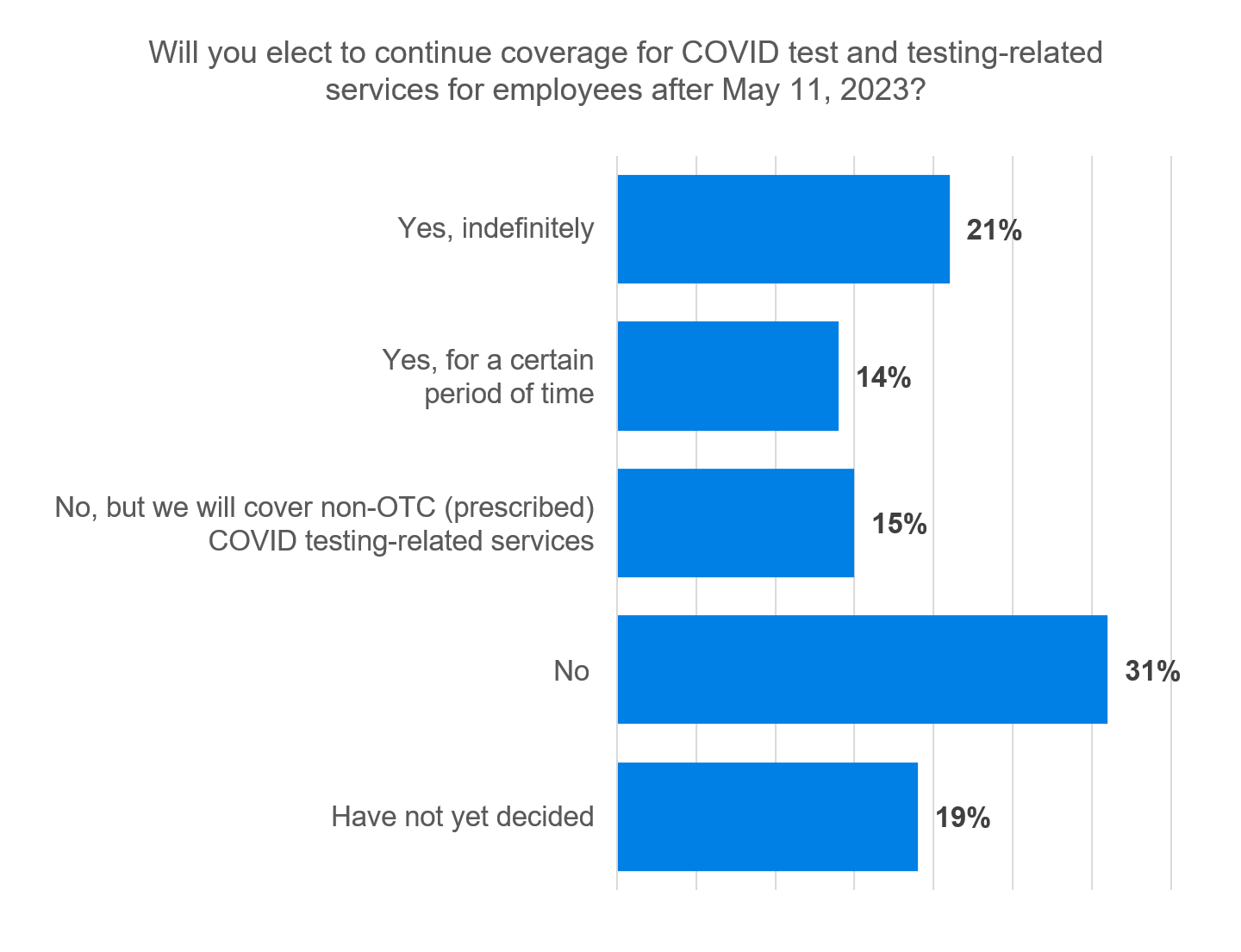
During the declared emergencies, employers were able to offer standalone telehealth benefits and other remote care services to individuals not eligible for coverage under any other group health plan offers by the plan sponsor. This coverage is ending with the expiration of the federal emergencies.
Most respondents (62%) indicated that they did not take advantage of this opportunity to broaden access to telehealth services within their populations. Consequently, the lifting of this coverage eligibility will not impact their plans.
Communications
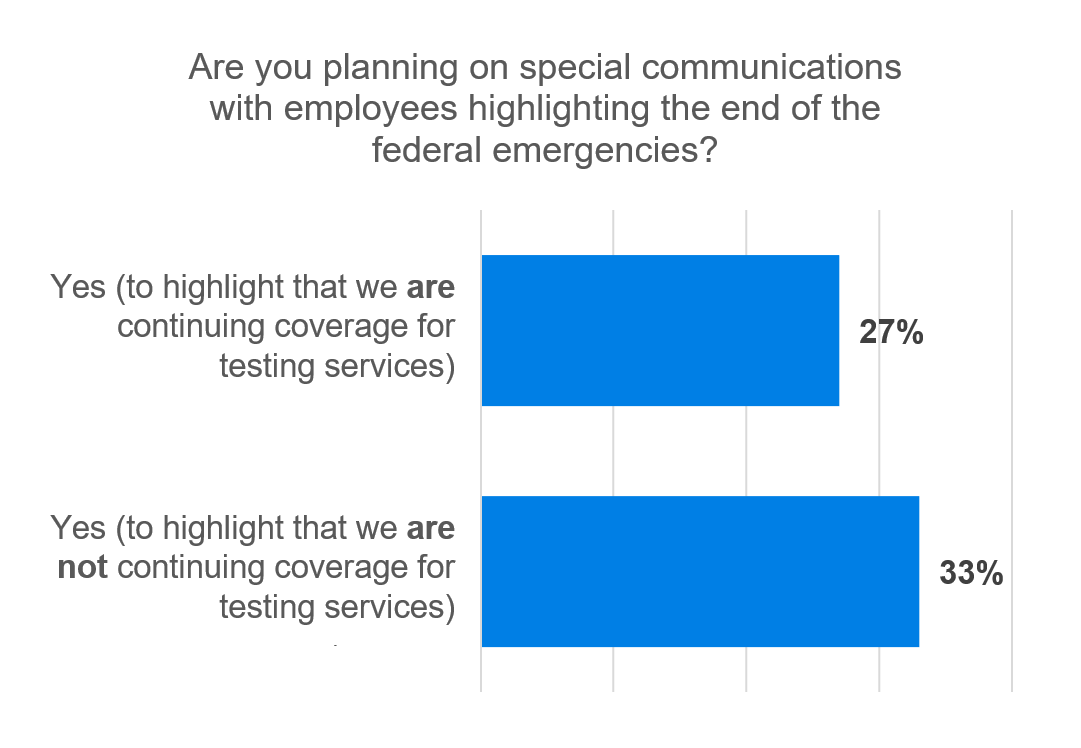
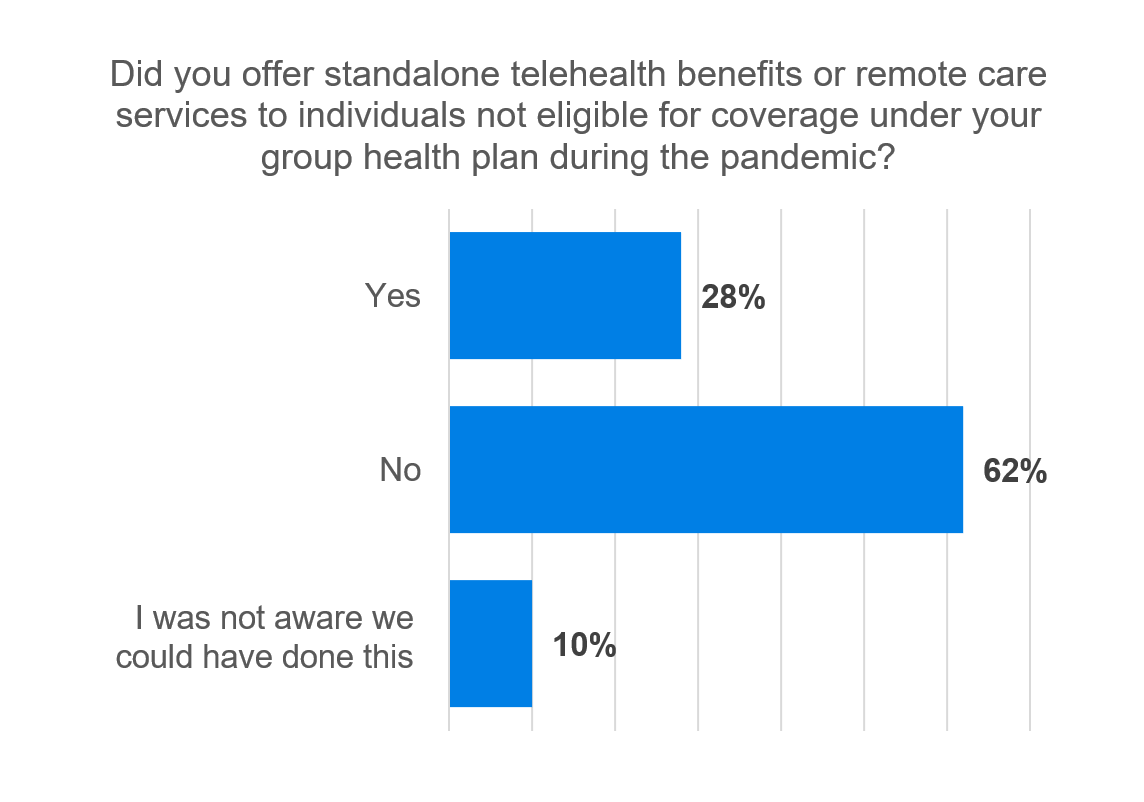
Employers are preparing communications to detail what is changing for employees and their dependents. One might think that employers would want to prepare communications just to promote the continuation of coverage with employees. However, respondents to our Pulse Survey indicated that they are choosing to highlight both the continuation of coverage (27%) as well as not continuing coverage (33%).
Out of those respondents who indicated they were planning special communications, 31% were doing so as a requirement due to plan amendment or notification of material reduction in covered services. The other 69% of respondents were still planning these special communications although they are not required.
For those respondents choosing not to communicate with employees, their reasoning was clear. Nearly three-fourths of those respondents felt that employee communications “are not necessary” (75%). We also recognize that some of our respondents had not made determinations on whether they would communicate with employees.
Download the full results or listen
The results of this Pulse Survey were featured recently in a conversation on Milliman’s Critical Point podcast regarding the end of the federal emergencies and its impact on employers and plan sponsors. To access this episode and the entire catalog of past Critical Point podcasts, listen from your favorite podcast app or visit https://www.milliman.com/en/insight/critical-point-podcast.
Full details of this entire survey including comprehensive results for each response and participant demographics, visit our library of past Pulse Surveys on What's Trending in Benefits? at https://www.milliman.com/pulse-survey.
Request your own survey
Have a future What’s Trending in Benefits? survey topic that would be of value to your organization? Our database of employers and plan sponsors used in this research includes more than 5,000 organizations, ranging from 500 to 300,000 employees, across a broad spectrum of industries. Milliman surveys are an objective, unbiased, effective, and highly affordable approach to better understanding how your organization is strategically positioned in areas of importance to you within the market.
Caveats
This survey summary has been prepared for informational purposes only. Milliman does not intend to benefit or create a legal duty to any recipient of this summary.
1 At the time of this survey, both the Public Health Emergency and National Emergency were anticipated to expire on May 11, 2023. On April 10, 2023, President Biden signed a congressional resolution ending the National Emergency.
2 While the ACA mandated that group health plans and insurers must provider certain preventive services without cost sharing when delivered by an in-network provider, a federal judge struck down the ACA requirement on March 30. The interpretation as to what preventive services are subject to this ruling is ongoing. The Biden administration has challenged the decision and an appeal is ongoing.